Prior authorization (PA) is a process used by health insurance companies to determine whether they will cover a prescribed procedure, service, or medication. The goal is to ensure the proposed treatment is medically necessary and falls within the insurer's coverage guidelines.
Legacy technology and time-consuming manual processes associated with PA contribute to an estimated $950B in administrative costs and 94% of delays in patient treatment, with doctors spending upwards of 13 hours per week on PA.
Conducting research with a vast network of payers and providers, we partnered with Google Cloud and Myndshft to design and build NexAuth, a suite of AI-enabled services that can be integrated with existing PA workflows to cut costs, improve member and provider experiences, and expedite care delivery.
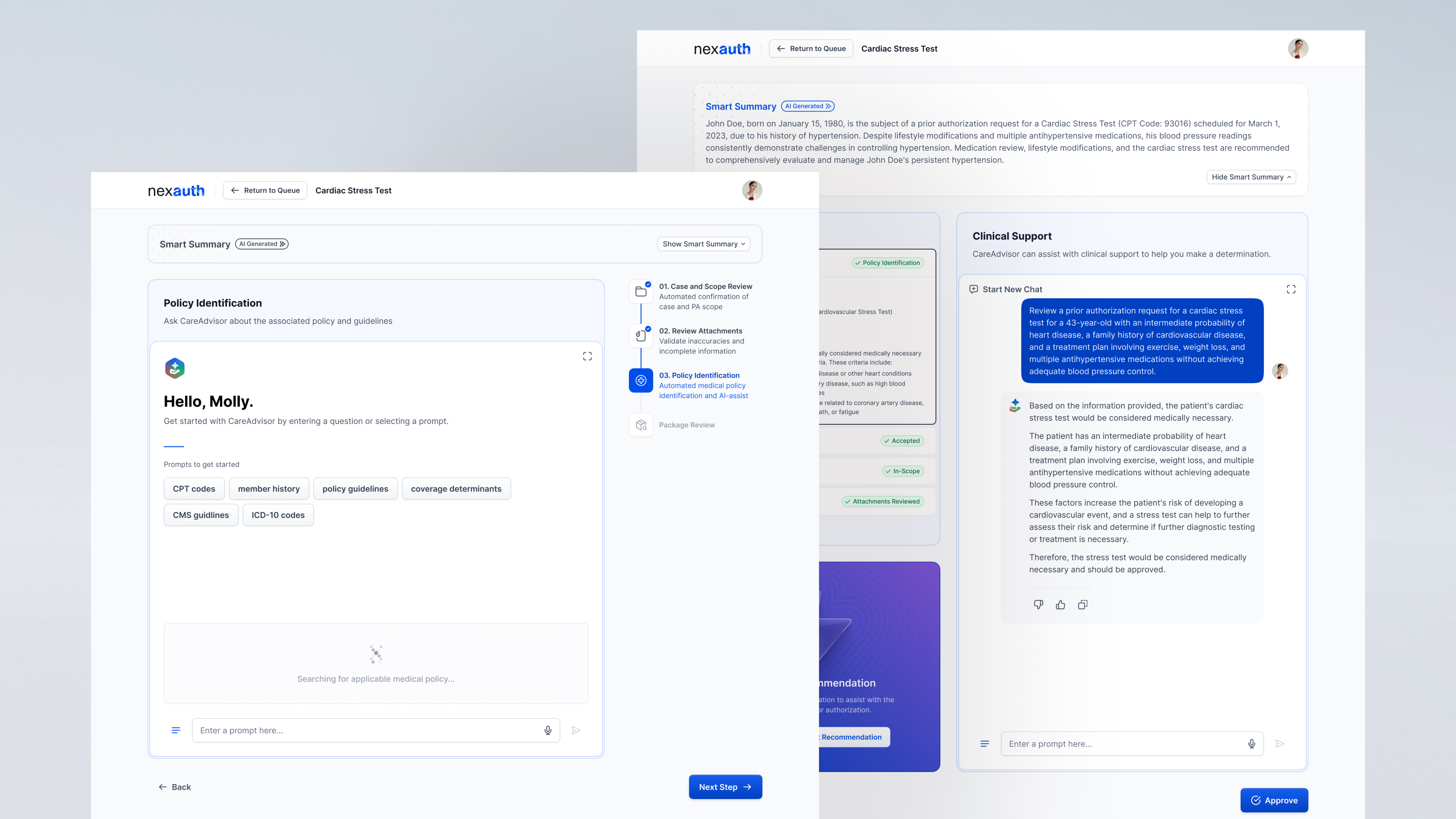
The current PA workflow has many steps, from checking a member’s eligibility to clinical review, decision, and notification. We interviewed stakeholders involved in all aspects of the PA process, including administrators, nurses, clinicians, and IT support, to develop a clear understanding of where AI could offer the most significant value.
Our decisions were guided by administrators and clinicians involved in the day-to-day processing of PAs. Administrators need to be able to quickly review and validate the accuracy of a PA request, while clinicians must interpret complex medical and policy guidelines associated with the request to make an approve/deny decision.
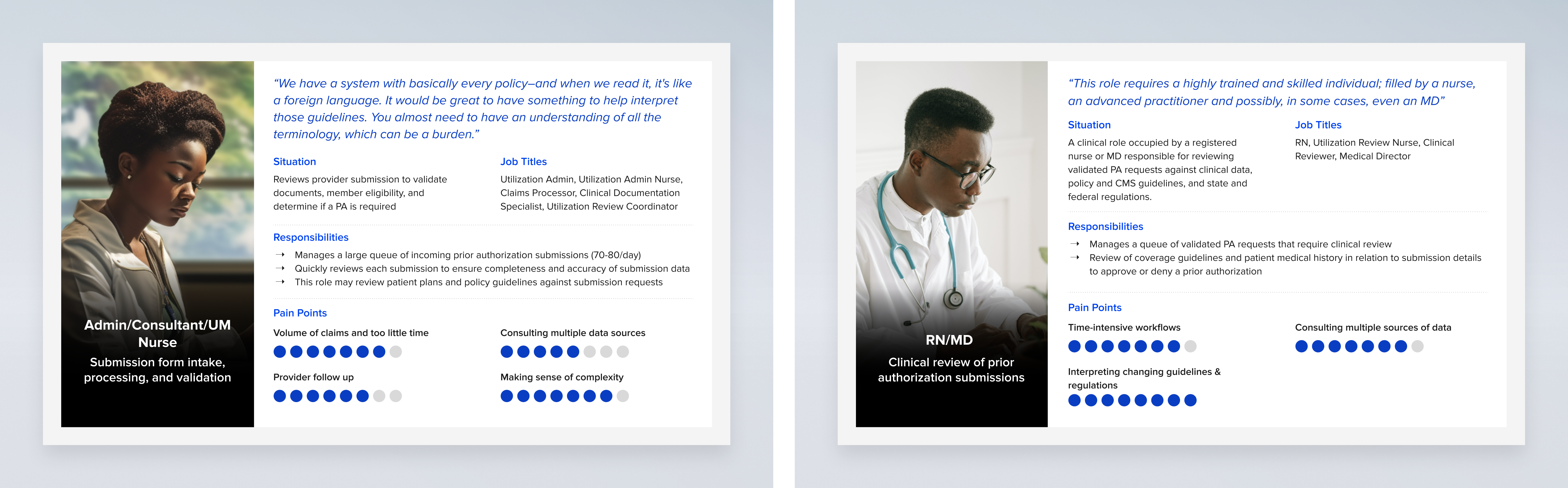
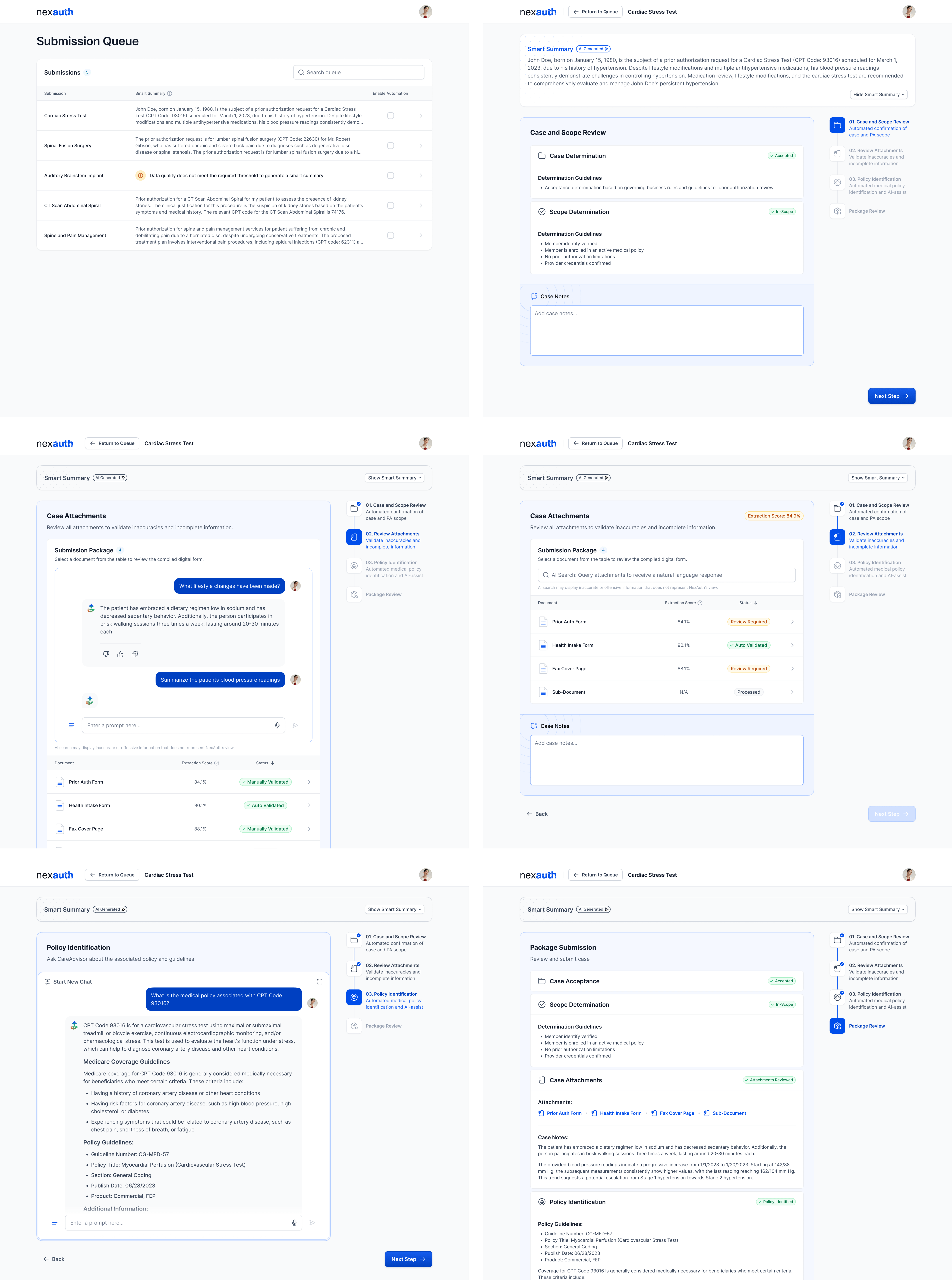
Understanding that many payers are in various stages of investing in automation capabilities, NexAuth integrates with current PA processes, allowing payers to gain the immediate advantages of AI, even as roadmaps continue to evolve. The solution offers payers four modular services:
Intake: Automates document processing, turning forms into structured data that’s easily accessible through an intuitive conversational interface.
Case Validation: Uses algorithms to verify coverage across 2,000+ payers with high accuracy.
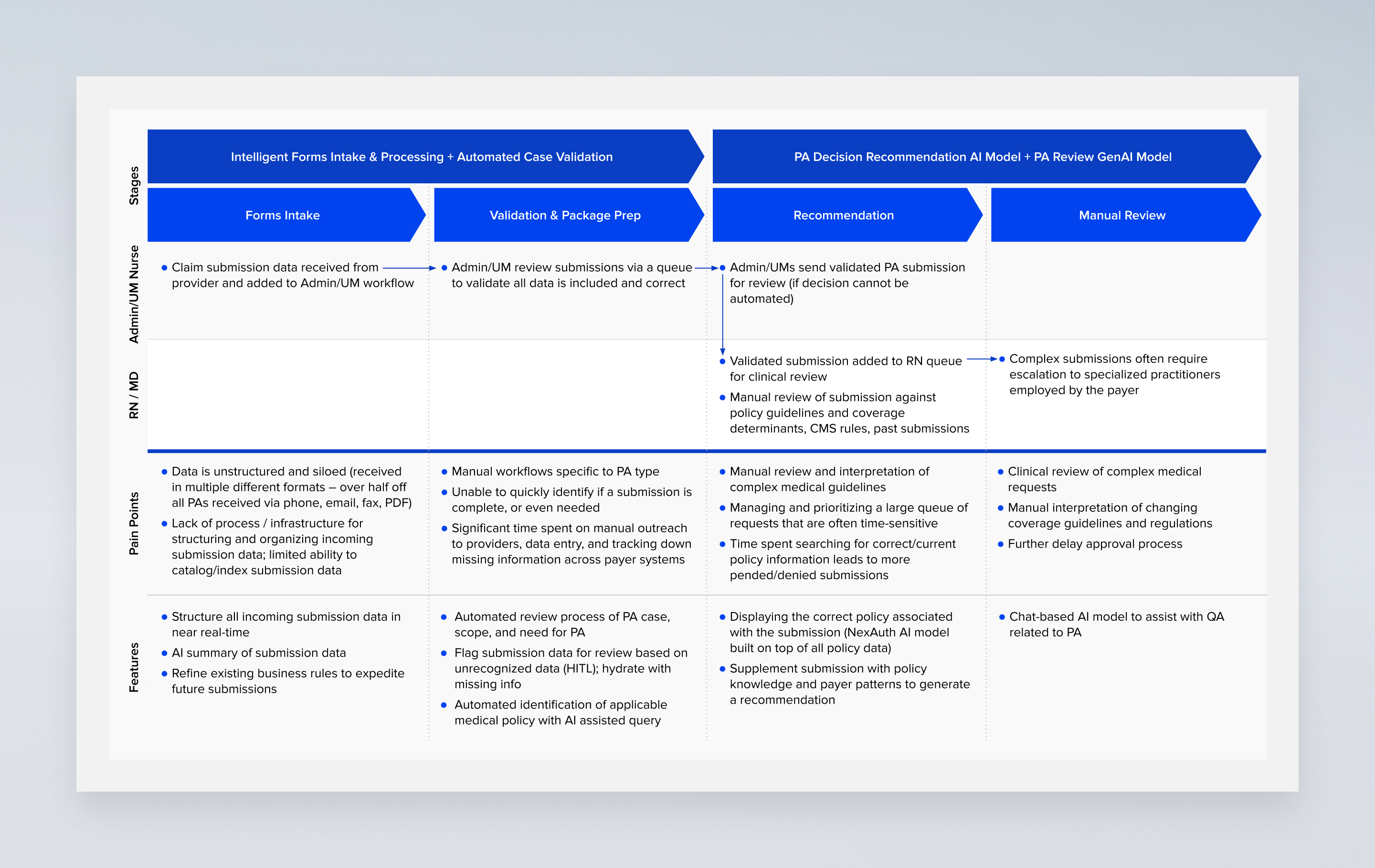
Clinical Recommendation: Supports complex cases by combining policy and medical history data to provide a personalized approve/deny recommendation.
Clinician Review: Clinicians get an extra layer of support, enhancing decision-making via a conversational interface.
While NexAuth’s Intake and Case Validation services are focused on freeing up staff, particularly nurses and clerical personnel performing data entry, Clinical Recommendation and Review will automate most PA decisions leaving complex and sensitive decision-making to experienced clinicians. While these features offer considerable benefits, it's crucial to acknowledge and address the substantial ethical, safety, and trust considerations that come with integrating AI into healthcare, ensuring that such innovations enhance rather than compromise patient care and data integrity.
With that in mind, NexAuth is engineered to streamline efficiency while maintaining a transparent user experience that gives users visibility and oversight during each step of the PA workflow. The experience guides users through a sleek, intuitive interface, where crisp, engaging interactions are complemented by instant feedback and contextual support, ensuring a seamless and user-friendly journey.